Philadelphia woman used Counterforce Health to Appeal Health Insurance Denials

Health insurance claim denials affect millions of Americans annually, with nearly one in five insured individuals experiencing coverage rejections for essential medications and treatments. However, a groundbreaking AI platform called Counterforce Health is revolutionizing how patients fight back against these denials, turning a traditionally complex and time-consuming process into a streamlined, two-minute solution.
What is Counterforce Health?
Counterforce Health represents a cutting-edge artificial intelligence platform specifically designed to generate customized insurance appeal letters. This innovative tool leverages advanced AI technology to analyze patient insurance details, aggregate medical research, and utilize databases of successful appeals to create compelling, evidence-based arguments for coverage approval.
Unlike traditional manual appeal processes that can consume 8-10 hours of research and writing, Counterforce Health's AI system delivers comprehensive appeal documentation in under two minutes, making it an invaluable resource for patients navigating complex insurance bureaucracy.
Real-World Success
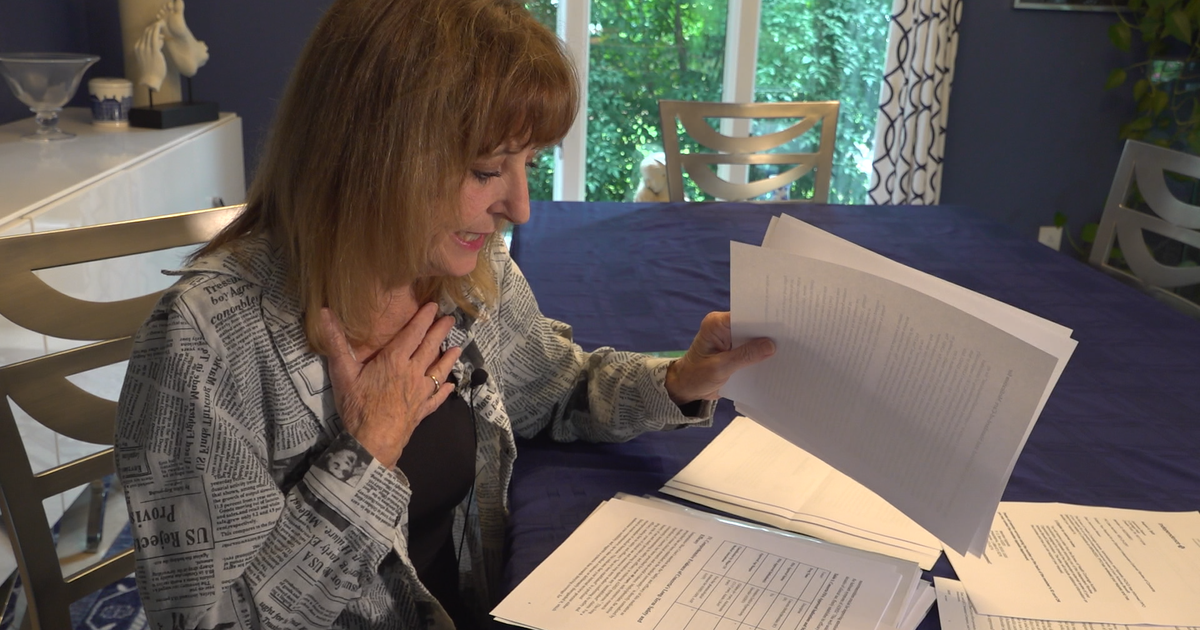
The effectiveness of Counterforce Health was recently demonstrated in a compelling case involving Joani Reisen, a Delaware County businesswoman whose health insurance provider suddenly discontinued coverage for her essential ADHD medication, Concerta (methylphenidate). After relying on Concerta (methylphenidate) for over a decade to manage her ADHD and operate her e-commerce business, Reisen faced a devastating coverage denial from Independence Blue Cross (IBX). The insurance company classified her medication as "experimental," forcing her to consider generic alternatives that proved ineffective, causing drowsiness and inability to function professionally.
Traditional appeal attempts through her physician failed twice, leaving Reisen frustrated and medication-free. This scenario reflects a broader healthcare crisis where patients lack the resources, knowledge, or time to effectively challenge insurance denials.
When conventional approaches failed, Reisen turned to Counterforce Health for her third appeal to Pennsylvania's Insurance Commission external review panel. The AI platform generated an impressive 11-page appeal letter featuring:
- Comprehensive medical research citations
- Hyperlinked supporting documentation
- Evidence-based arguments against the "experimental" classification
- Tailored content specific to her insurance provider and situation
The result? A successful appeal that restored her medication coverage.
Why Counterforce Health Works?
Advanced AI Training and Database Integration
Counterforce Health's effectiveness stems from its extensive training on tens of thousands of successful insurance appeals. This comprehensive database enables the AI to:
- Identify winning strategies for specific medications and conditions
- Understand insurance company patterns and preferences
- Generate evidence-based arguments using current medical literature
- Customize appeals based on individual patient circumstances
Addressing the Appeal Gap
Research from the Kaiser Family Foundation reveals a critical healthcare challenge: fewer than 1% of denied insurance claims are appealed by patients. However, when appeals are submitted, they succeed in 44% of cases, demonstrating the untapped potential for successful coverage restoration.
This appeal gap exists because patients typically:
- Lack knowledge about their appeal rights
- Cannot invest the substantial time required for manual research
- Don't understand the complex medical and legal language needed
- Feel overwhelmed by insurance company bureaucracy
Advantages of the AI Tool
Time Efficiency Revolution
What traditionally requires 8-10 hours of manual research, medical journal analysis, and database searching is completed in under two minutes through AI automation.
Research-Backed Arguments
The platform accesses vast medical databases and research repositories to provide scientifically sound justifications for coverage requests.
Accessibility and Cost
Counterforce Health operates as a free service, supported by grants from prestigious institutions including the National Institutes of Health and the University of Pennsylvania.
Co-founder and chairman Neal Shah envisions making insurance appeals as simple as online shopping, removing technical barriers that prevent patients from advocating for their healthcare needs. The development of Counterforce Health stems from personal experience with healthcare system challenges. Shah's motivation comes from navigating complex insurance appeals while caring for his wife during her cancer treatment, understanding firsthand the frustration and urgency patients face when coverage is denied.
Impact on Healthcare Accessibility
Counterforce Health addresses a fundamental healthcare equity issue by democratizing access to effective appeal resources. Previously, successful insurance appeals often required expensive legal representation or extensive medical knowledge. This AI platform levels the playing field, providing sophisticated appeal capabilities to any patient with internet access.
The Future of AI in Healthcare Advocacy
As artificial intelligence continues advancing, tools like Counterforce Health represent the future of patient advocacy. The platform's success suggests broader applications for AI in healthcare navigation, potentially transforming how patients interact with insurance systems, understand their rights, and access necessary treatments.
The integration of AI into healthcare appeals processes signals a shift toward patient empowerment, where technology serves as an equalizer against complex institutional barriers. As more patients discover and utilize these tools, insurance companies may need to reconsider denial practices when facing consistent, well-researched appeals.
Empowering Patients Through AI Innovation
Counterforce Health demonstrates how artificial intelligence can serve as a powerful ally in healthcare advocacy. By transforming the insurance appeal process from a daunting, time-intensive challenge into an accessible, evidence-based solution, this platform empowers patients to fight for the coverage they deserve.
For patients facing insurance denials, Counterforce Health offers hope, efficiency, and proven results. As one successful user noted, "Everybody should know about it" – a sentiment that reflects the transformative potential of AI-powered healthcare advocacy tools.
Ready to fight your insurance denial? Counterforce Health's free AI platform could be the key to restoring your essential healthcare coverage in just minutes.
Learn More: