Counterforce Health Featured in National Stateline's Coverage of AI in Healthcare
We're proud to announce that Counterforce Health was recently featured in Stateline's groundbreaking investigative article "AI vs. AI: Patients deploy bots to battle health insurers that deny care." The piece, published by one of the nation's most respected sources for state policy reporting, shines a spotlight on how patients and healthcare providers are leveraging artificial intelligence to fight back against an increasingly automated insurance denial system.
The Growing Crisis in Healthcare Claims
The Stateline investigation reveals a troubling trend that's been accelerating across the American healthcare landscape. As more health insurance companies turn to AI to automate claims processing and prior authorizations, the share of denied claims has risen dramatically. According to a September 2024 report from Experian cited in the article, 41% of physicians and other healthcare providers now report that their claims are denied more than 10% of the time—a significant jump from just 30% three years ago.
The numbers are even more stark when you look at specific insurance marketplaces. Insurers on Affordable Care Act marketplaces denied nearly one in five in-network claims in 2023, up from 17% in 2021. For out-of-network claims, more than a third are being denied. These aren't just statistics—they represent real patients facing barriers to getting the care their doctors have prescribed.
Major insurance companies have come under intense scrutiny for their use of algorithms. The article highlights how UnitedHealth Group has faced criticism from media outlets and federal lawmakers for allegedly using algorithms to systematically deny care to seniors, while Humana and other insurers face lawsuits and regulatory investigations over their use of sophisticated algorithms to block or deny coverage for medical procedures.
Empowering Patients in the Appeals Process
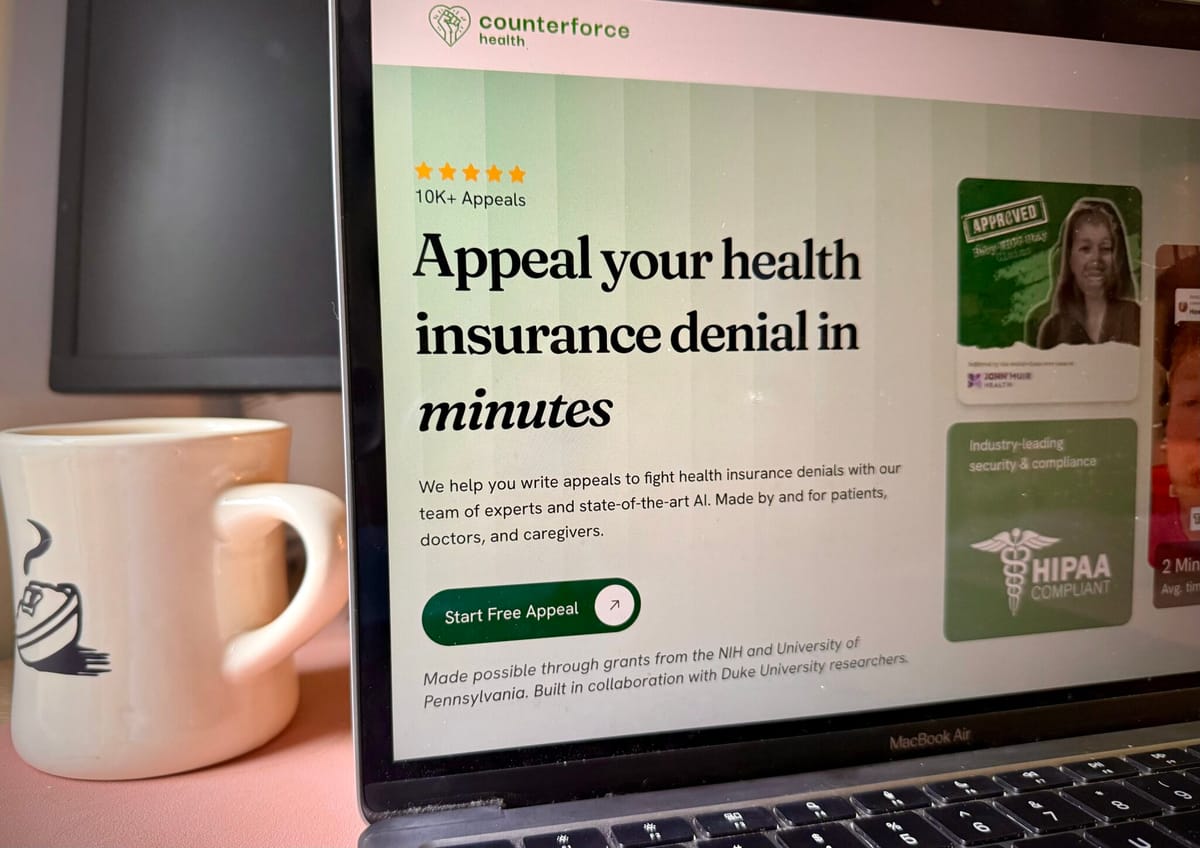
This is where Counterforce Health enters the picture. As featured in the Stateline article, we've developed a free AI assistant specifically designed to help North Carolina patients appeal denied health insurance claims and fight large medical bills. Our service uses advanced AI models to carefully analyze a patient's denial letter, then examines both the patient's specific insurance policy and relevant medical research to draft a customized, compelling appeal letter.
The article recognizes Counterforce Health as part of a growing movement of consumer-focused AI tools that are helping to level the playing field between patients and insurance companies. While insurers deploy AI to rapidly process and deny claims, patients now have access to technology that can help them understand their rights and fight back effectively.
Why Appeals Matter and Why They're So Rare
One of the most striking statistics highlighted in the Stateline piece comes from a KFF analysis: fewer than 1% of health coverage denials are ever appealed. This is a staggering figure that reveals just how intimidating and inaccessible the appeals process has become for ordinary patients. Even when patients do muster the courage and resources to appeal, they lose more than half of those appeals.
Why don't people appeal? The healthcare system has become a "black box," as the article describes it. Understanding why a claim was denied, what your policy actually covers, and how to construct an effective appeal requires navigating byzantine bureaucracy, deciphering complex medical and insurance jargon, and investing significant time and energy, often while dealing with health challenges.
New consumer-focused AI tools like Counterforce Health have the potential to shift this dynamic by making appeals easier to file and the process more transparent and understandable. By automating the analysis of denial letters and policy documents, and by drawing on medical research to support appeals, we're removing many of the barriers that have historically prevented patients from advocating for themselves.
The Human Element Remains Critical
The Stateline article doesn't just celebrate technology, it also raises important questions about the role of human oversight. As Harvard Law School's Carmel Shachar points out in the piece, "It doesn't feel like a satisfying outcome to just have two robots argue back and forth over whether a patient should access a particular type of care."
This concern resonates with our approach at Counterforce Health. While AI can be incredibly powerful for analyzing documents, identifying relevant policy language, and drafting initial appeal letters, we recognize that healthcare decisions are deeply personal and the stakes are extraordinarily high. The article notes that without human oversight, AI tools are vulnerable to mistakes, including "hallucinations" where the AI might generate plausible-sounding but inaccurate information.
We've designed our service with these limitations in mind, providing patients with tools that enhance their ability to advocate for themselves while encouraging them to review and understand the appeals we help them create. As one patient featured in the article noted, "AI in and of itself isn't an answer. AI, when used by a professional that understands the issues and ramifications of a particular problem, that's a different story."
A Nationwide Movement for Patient Advocacy
The Stateline article places Counterforce Health within a broader ecosystem of patient advocacy tools. Companies like Sheer Health are offering apps that help consumers connect their insurance accounts, upload medical bills, and get answers about deductibles and copays. Other services focus on catching billing errors or translating medical jargon into plain English.
This movement comes at a critical time. The article reports that a quarter of adults under age 30 now use AI chatbots at least once a month for health information or advice, showing both the demand for accessible healthcare guidance and the trust younger generations are placing in AI technology.
Meanwhile, states across the country are racing to regulate AI in healthcare. More than a dozen states have already passed laws this year governing how insurers, physicians, and others can use AI. Arizona, Maryland, Nebraska, and Texas have gone so far as to ban insurance companies from using AI as the sole decision-maker in prior authorization or medical necessity denials.
Our Mission Moving Forward
Being featured in Stateline validates our mission and reinforces our commitment to making healthcare more accessible and fair. We built Counterforce Health because we believe that everyone deserves a fighting chance when their insurance company denies coverage for care their doctor has recommended. The complex, opaque nature of health insurance shouldn't be a barrier to getting the treatment you need.
As the article makes clear, this is just the beginning of a larger transformation in how patients interact with the healthcare system. While insurers have been quick to adopt AI for processing claims, patients are now arming themselves with similar tools to ensure their voices are heard and their rights are protected.
We're honored to be part of this story and grateful to Stateline for highlighting the important work being done to help patients navigate an increasingly complex healthcare landscape.
Read More and Get Help
You can read the full Stateline article, "AI vs. AI: Patients deploy bots to battle health insurers that deny care," on their website. If you've received a denial letter from your health insurance company, we encourage you to try Counterforce Health's free AI assistant. Together, we can fight for the care you deserve.
Counterforce Health is a North Carolina-based nonprofit dedicated to helping patients appeal denied insurance claims and navigate complex medical bills. Our free AI-powered service is available to anyone who needs help understanding their rights and fighting for their healthcare.
Original Article: https://stateline.org/2025/11/20/patients-deploy-bots-to-battle-health-insurers-that-deny-care/
